
FOREWORD

Syed Munir Khasru
Chairman
Institute for Policy, Advocacy, and Governance (IPAG)
As the world moves in a post-pandemic world, it is important that leaders, thinkers, and doers reflect on our deep-rooted shortcomings that the COVID-19 pandemic has brought to the surface. Besides the socio-economic disruption and resulting stress, COVID-19 has tested both the economies and healthcare systems across the globe. Being resource constrained, developing countries experienced the chaos on a different note.
Following the pandemic, there have been at least 7–13 million excess deaths worldwide of which possibly 86% occurred in developing countries. It comes as no surprise that flattening the curve has been challenging for developing countries, considering the unplanned urbanization, dense population and resulting congestion. It does not help to know that at least 1 billion people live in slums.
Consequently, SDG 3, Good Health and Well-Being, has been severely hit because of its interconnected nature with other goals like SDG 1 (Poverty), SDG 2 (Zero Hunger), SDG 4 (Quality Education), SDG 5 (Gender Equality), SDG 6 (Clean Water and Sanitation), SDG 13 (Climate Action), SDG 14 (Life under Water), SDG 15 (Life on Land) and SDG 17 (Partnerships for the Goals). Like a vicious circle, the pandemic has aggravated the systematic inequality plaguing the developing countries and hampering all the components which ensure people’s good health and well-being. Since 119–124 million people, especially from developing countries were pushed back into poverty, years of hard work revolving around the 2030 Agenda for Sustainable Development has been reverted.
For instance, in 2021, as 9.3 million jobs were lost, COVID pushed 4.7 million people in Southeast Asia back into extreme poverty.
Additionally, disruptions in health services have amplified due to the pandemic, in turn, worsening the situation in developing countries. Initially, around 70 countries had paused childhood vaccination drives. Health services such as cancer screening and family planning were forced to take a backseat as the world focussed on curbing the pandemic. In the first wave of the pandemic, South Asian countries were grappling with their faltering healthcare systems, because of which 11,000 mothers and 228,000 children in the region died.
These disruptions risk undoing years of development in the global healthcare system. For enhanced response to the future crisis, putting SDGs at the centre of recovery plans is extremely essential. Henceforth, involving resilient health systems, green recovery, working towards gender parity and a healthier environment should be the priority. Leaders and governments must feel obliged to make the most out of this situation and work on restricting and improving the way in which we address sustainable development and resiliency.
Against the above global background, this report highlights how the pandemic has further derailed the period of SDG implementation from the “Decade of Action”, especially delving into the impact on SDG 3. It also provides valuable insights into the overall SDG ecosystem in light of the worst pandemic in recent living memory.

Since COVID-19 emerged as a global health emergency in early 2020, it has had a domino effect on the progress made in terms of the Sustainable Development Goals, especially SDG 3: Ensure healthy lives and promote wellbeing for all at all ages, further stalling the progress of Universal Health Coverage. By mid-2022, 500 million people were infected with the SARS-CoV-2 virus worldwide, leading to at least 15 million deaths between 2020–2021. Immunization rates fell in 2020, 22.7 million children missed out on basic vaccines (3.7 million more children in comparison to 2019). COVID-19 had tested the healthcare systems of 92% of countries across the world by 2021, claiming the lives of at least 115,500 front-line workers involved in healthcare.
The Sustainable Development Goals Report 2021 indicated how progress made toward achieving SDGs has either slowed down or regressed due to COVID-19. In 2020, approximately 119–124 million people fell into poverty while the number of people suffering from hunger surged to 132 million. Further, around 255 million people lost their full-time jobs. In addition, the reading proficiency of at least 101 million youth and children worldwide had dropped below the minimum level, challenging the achievements made in the last 20 years.
With multiple supply chains disrupted and developed countries hoarding vaccines, the stark inequality in our world exacerbated. At present, there are 2.6 billion people awaiting their first dose of vaccination against COVID-19. Ensuring equitable distribution of basic access to services such as sanitation, clean drinking water, and electricity goes hand in hand with maintaining SDG 3. Hence, the pandemic not only threatens good health and well-being but also its predetermining counterparts, placing the progress of all 17 SDGs at imminent risk.
The pandemic has exposed the cracks in even the world’s strongest healthcare systems and their economies, implying how there is always room for improvement. Thus, this post-pandemic backdrop is a golden opportunity for placing sustainability at the forefront whilst dealing with matters of global urgency. To undo the damage of COVID-19, we need to ensure that no one is left behind and the 2030 Agenda for Sustainable Development is enshrined into government strategies of developed, developing, and underdeveloped countries.
Introduction
Prior to the onset of the pandemic, SDG 3 (Good Health and Well-Being) targets seemed promising and quite feasible as the world was progressing remarkably toward improving the health and overall wellness of the population. Millions of people from across the world including those living in developing countries across Asia had benefited from the ongoing improvements. Some notable pre-pandemic global progresses include increase in life expectancy, declining trends of child mortality and maternal mortality, and decrease in non-communicable diseases (NCDs).
On a global scale, there was a decline in under-5 mortality rate, falling to 39 deaths in 2017, immunization against pertussis, tetanus, and diphtheria rose to 85% in 2017 from 72% in 2000. Similarly, between 2015 to 2017, administering of the second dose of vaccines for measles climbed from 59% to 67% in 2017.
Since early 2020, the pandemic has exposed the weakness in the healthcare system of several countries within Europe, the Indian Subcontinent, and Southeast Asia. As the SARS-CoV-2 virus has mutated into stronger and severely contagious variants, the existing challenges regarding SDG 3 and Universal Health Coverage (UHC) have aggravated to an extent where countries are unable to deal with the virus alone. COVID-19 places the progress of the SDGs at risk of not meeting targets, especially SDG 3.
This report concisely presents the overall impact the COVID-19 pandemic has had over SDG 3 and how, in turn, it has impacted health coverage, rate of diseases, and treatment of communicable diseases and NCDs within South Asia, Southeast Asia, and Europe.
Conceptual Framework
The World Health Organization (WHO) meticulously designed the Universal Health Coverage (UHC) framework, with 16 indicators placed under four categories, i.e., reproductive, maternal, newborn and child health, infectious diseases, noncommunicable diseases, service capacity and access. The UHC is already positioned by WHO as a strategic and research-based goal, aspiring to reach at least 1 billion people by the end of 2023. Additionally, targets from SDG 3: Good Health and Well-Being have been used as an indicator for determining progress or regression. Thus, findings for the report were obtained and analyzed whilst applying UHC and SDG 3 as a conceptual framework for chalking out the process of the research.
Methodology
The primary method of research adopted for this report was content analysis which was conducted by drawing references from a plethora of literature. The approach was combined with inductive reasoning to further comprehend, validate, and make sense of empirical data which were obtained from reliable secondary sources. Indicators under the UHC framework were considered as dependent variables whereas the COVID-19 pandemic was considered as the independent variable.
Between November 1, 2021 and April 1, 2022, we identified trends in healthcare through statistical reports, newspaper articles, research articles, and journal publications from well-reputed sources. Data was gathered and sectioned according to indicators and region for better understanding.
Empirical data on the impact of COVID-19 were obtained and juxtaposed with SDG 3 targets to analyze whether there was a correlation between the pandemic and the rate of progress of SDG 3. Therefore, data was sifted and processed as per the SDG 3 indicators. The area of study chosen for this report were South Asia, Southeast Asia, and Europe. Sampling was purposive as study population considered for the research were strictly confined to the two regions.
Findings
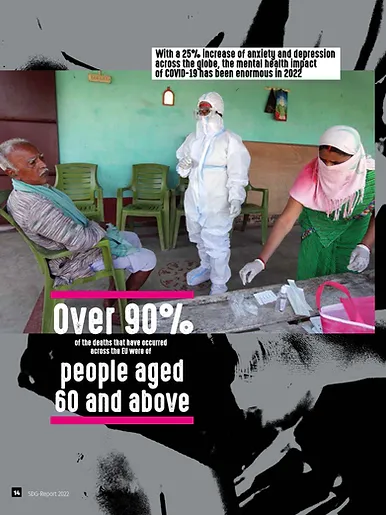
The COVID-19 pandemic has disproportionately contributed to excessive mortality rates. End of March 2022 almost 6.2 million people have died worldwide after getting infected with the virus. Over 90% of the deaths that have occurred across the EU were of people aged 60 and above. In South Asia every minute three people died due to COVID.
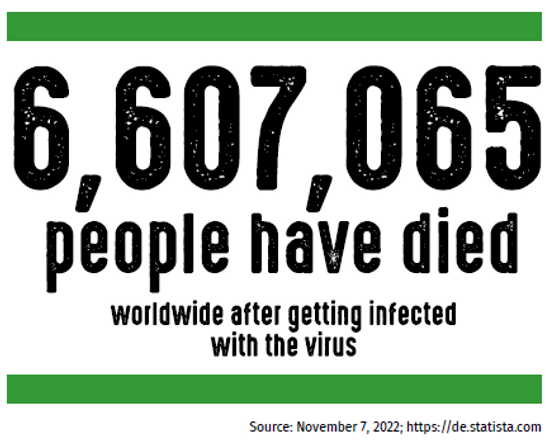
For instance, in India, 521,000 deaths have occurred among 43,000,000 cases. In Southeast Asia, the Philippines and Indonesia reported some of the highest COVID-19 deaths per million standing at 24.47 and 22.69 respectively. The Johns Hopkins University reported that as of August 2021, Southeast Asia reported one of the world’s highest death tolls in effect of the delta variant with an excess of 38,522 deaths. To delve deeper into the impact COVID-19 has had on the progress of SDG 3, we have selected a few targets as indicators of progress.
Target 3.3: Ending Epidemics
The pandemic had stalled the efforts to spread immunization through the polio vaccine campaigns
worldwide in 2020. Lockdown measures, social distancing, and disruption in transportation and logistics ultimately led to the suspension of campaigns, impacting the developing south disproportionately.
In 2020, despite global coverage of measles vaccine standing at 87%, much below the 95% target, 25 countries including countries in Europe, Southeast Asia, and Asia had suspended measles vaccine campaigns, placing 80 million children at risk of dying from measles. France, Italy, UK, Germany, and Spain are among the top 10 high income countries with the highest levels of children who have not been administered the first dose of measles vaccine. Similarly, in the same year, Southeast Asia experienced a drastic decline in diphtheria, tetanus toxoid and pertussis (DTP3) immunization, at least 57% where eight of the eleven countries reported disruptions in routine immunization.
Cases for tuberculosis (TB) have been underreported since the onset of the pandemic as social distancing measures and reshuffling of resources toward COVID-19 posed as a limitation for case finding TB diagnosis. TB cases notifications have plummeted by 18% between 2019 and 2020, standing at 5.8 million. People seeking treatment for MDR/RR-TB fell by 15% and TB preventive treatment fell from 3.6 million to 2.8 million. India, Bangladesh, Indonesia, Philippines, and Ukraine have been among the largest contributors to underreporting TB cases in 2020.
Target 3.4: Non-communicable Diseases, and Mental Health and Well-Being
Though pre-mature death from non-communicable diseases accounts for approximately 41,000,000 of the deaths, measures taken for treatment have drastically fallen in Europe, South Asia, and Southeast Asia. In Europe, screening rates of cervical cancer and breast cancer fell to -55% and -54% respectively in the first quarter of 2020 in Italy and remained persistently low for the rest of the year. In Czech Republic, colorectal cancer screenings declined by 58% in 2020 whereas in Austria, it dropped by 34%.
In 2020, only 20% of countries from the Southeast Asian Region reported that they have allocated additional fundings for NCDs. A majority of the countries have refocused their strategic plan of action toward COVID-19. However, 66% of countries including Southeast Asian countries ensured that the NCD services were recognized as an essential health service in their national COVID-19 response plan. While an approximate of 70% European countries reported using triaging to treat NCDs, only 10% of South Asian and Southeast Asian countries resorted to triaging. There are also discrepancies in percentages of countries collecting data on NCD comorbidities in patients with COVID-19 with 88% of European countries collecting data and only 40% of South Asian and Southeast Asian countries combined.
With a 25% increase of anxiety and depression across the globe, the mental health impact of COVID-19 has been enormous in 2022 due to several factors such as illness, deaths, loss of education, financial insecurity, panic, and unemployment among others. Moreover, an absence of social connections due to lockdown measures also contributed to poor mental health. As of 2021, COVID-19 has led to the disruption of essential mental health services across 93% countries worldwide. Governments
around the world accommodated a meagre 2% of their health budget for mental health. In fact, several developing countries have reported that less than 1 healthcare worker focusing on mental health per 100,000 people.
During the peak of COVID-19 infections in Europe, cases of anxiety and depression doubled in UK, France, and Belgium. The Netherlands was one of the European countries to report the poorest mental health during the initial stages of the pandemic with one third of its population reporting feelings of anxiety, loneliness, and stress, and 20% facing difficulty in their sleep patterns. Likewise, in Belgium, depression and anxiety jumped from 11% in 2018 to an average of 23%. In Southeast Asia, approximately every 1 in 3 young people in Indonesia experienced depression or loss of interest in activities. As of September 2021, in Thailand, 32% of adolescents were at risk of depression, 28% experienced elevated levels of stress, and 22% experienced suicidal ideation. Higher prevalence of anxiety and depression linked to COVID-19 was found in India, Bangladesh, and the Maledives. Even in 2022, around 36% of the urban population in Bangladesh continued to experience anxiety due to COVID. However, there is a gap in notification of mental health cases, especially in South Asia.
Target 3.1 and 3.7: Universal Access to Reproductive Healthcare and Global Maternal Mortality Ratio
COVID placed pregnant people at serious risk of developing severe symptoms in comparison to people who were not pregnant. COVID also led to an increase in severe maternal mental health issues such as clinical depression and anxiety. As resources were concentrated towards controlling the pandemic, incidence of prenatal care visits decreased. Due to educational facilities being shut down for a prolonged period of time, the COVID-19 pandemic has placed an additional 10 million girls in danger of child marriage. Early marriages are indicative of complications during childbirth which may tamper the progress made in terms of maternal mortality ratio. In several low-income countries, there has been a significant decrease in antenatal care. For instance, in Bangladesh, antenatal care visits fell by 31% and skilled assisted deliveries fell by 2/3. In South Asia, COVID-19 may have caused an approximate of 11,000 additional maternal deaths.
Moreover, an estimate of 4.5 million girls in South Asia are unlikely to return to school and are in imminent danger of losing access to sexual and reproductive health services and information. Supply of contraception has been disrupted in India with a 21% decrease in IUD insertion, a reduction by 36% in injectable contraception, 28% decrease in abortions, and a reduction in condoms and oral contraceptive pills by 23% and 15% respectively. Southeast Asia faced similar difficulties. In 2020, maternal mortality was projected to rise by 44%–65% by a year in Vietnam following COVID-19. Additionally, clinical
and non-clinical family planning methods decreased by 20% and 10% respectively. In Malaysia, limitations
of reproductive health services during the pandemic have contributed to the average teenage pregnancy rate of 50 per day. Besides, at least 6 newborns have been abandoned since the inception of the pandemic and the imposition of the Movement Control Order in March 2020.
COVID has also tested some of the strongest healthcare across Europe. For instance, due to the pandemic, the UK had to withdraw 85% of its funding to UNFPA’s work for reproductive health. In Italy, several women faced challenges while seeking an abortion as lockdown restrictions exacerbated accessibility as some women missed the 90-day window time for an abortion and also had to face a mandatory waiting period of 7 days. Additionally, 5 out of 20 regions in Italy allow outpatient services for medical abortion.
Target 3B: Equity and Research & Development of Vaccines
At present, 35 vaccines have been approved for use worldwide, 17.8 billion doses have been secured, and
1.40 billion doses have been shipped by COVAX to 145 countries. However, there is a gaping difference
in pricing ranging from 2 to 40 USD per dose. Though the WHO has set a target for 70% immunization across the globe, vaccine inequity continues to persist with unequal distribution of doses among high-income and low-income countries. Trillions of dollars are to be lost through the global economy if vaccine equity is not established adequately. Despite 10.5 billion vaccine rollouts worldwide, only 13% have reached low-income countries compared to the 70% in developed countries.
There are discrepancies in first-dose vaccination rates among Europe, Southeast Asia, and South Asia. As of 2022, Bangladesh, India and Nepal have a vaccination rate of 78.2%, 72%, and 76.8% respectively. Thailand, Indonesia, Vietnam, and the Maldives vaccination rates are 79.5%, 72.5%, 82.8%, and 75% respectively. In Europe, Ukraine, Belgium, United Kingdom, and Italy have vaccination rates of 35.4%, 80.3%, 78.9%, and 84.1% respectively.
As of March 2021, the top recipients of the R&D funding for COVID-19 were Moderna Therapeutics (USA), Janssen (Belgium), Pfizer/BioNtech (USA), CureVac (Germany), Novavax (USA), AstraZeneca (UK and Sweden), Sichuan Clover Biopharmaceuticals (China), and Sinopharm (China) totaling approximately 4.891 billion USD. No companies from South Asia and Southeast Asia made the top list, implying that maximum expenditure of R&D for COVID- 19 vaccines is concentrated in the West and East Asia.
3C and 3D: Health Financing, Recruitment, and Strengthening Capacity of Developing Countries
The EU allocated a faction of the €37 billion from the EU budget to maintain and support the healthcare system as part of the Coronavirus Response Investment Initiative (CRII). Austria, Belgium, Denmark, France, and Germany were among the first 12 EU countries to receive the funding from the €672.5 billion recovery package for mitigating the risks and crises of the COVID-19 pandemic.
In South Asia, Bangladesh and Pakistan reported the largest healthcare coverage discrepancies due to wealth gap, recording a difference of 42.6 and 65.8 percentile respectively. In Bhutan, the health workforce is below WHO’s recommended ratio for human resources allocated to health services, standing at 0.5 doctors per 1,000 people. Furthermore, in India, the private sector constitutes for 78% of the care, focusing on curative and tertiary care. Overall, South Asia only utilizes 0.89% of its GDP for financing public healthcare infrastructures, a meagre amount in comparison to the global average of 5.8%. However, while response rates are not as swift as in Europe, countries are coming forward to strengthen healthcare infrastructure, capacity building in healthcare services, and facilitate an overall preparedness for national and global health risks. For instance, India has allocated 0.1% of its GDP for improving health infrastructure, testing facilities, isolation beds, ICU beds, and insurance coverage for healthcare workers among others.
Similarly, Sri Lanka has allocated 0.1% of GDP towards maintaining and improving its emergency response to health catastrophes. Bhutan has also partnered with the World Bank for a 5 million USD COVID-19 project, ensuring public health preparedness and pandemic response. In Southeast Asia, Indonesia’s healthcare system faced a massive burden in terms of excessive mortality, understaffed healthcare facilities, and inadequate medical supplies as a result of COVID-19. As of May 2020, in response to the pandemic, the government had converted four apartment towers into emergency hospitals to accommodate and treat around 24,000 COVID-19 patients.
The government of Malaysia responded to rising infections by designating 400 new sites including colleges, hotels, and public universities as quarantine zones across the country. In Thailand, a budget of 6.3 billion THB was approved for COVID-19 emergency response. Hospitals in Thailand were supplied with 1,000,000 surgical masks per day by the Ministry of Public Health.
As of 2022, the WHO reported that most of the countries in Europe, South Asia, and Southeast Asia had well developed capacity in terms of optimized health service data. Under “surveillance of public health threats”, most South Asian countries except for Nepal, Pakistan, and Afghanistan reported sustainable capacities, Norway, Austria, and UK in Europe reported sustainable capacities, and in Southeast Asia, Thailand, Vietnam, and Indonesia reported well-developed capacities. However, Europe has scored better than the Southeast Asian Region (South Asia and Southeast Asia combined) in the SCORE board.
IPAG Sources: https:⁄⁄www.care.at⁄sourcessdg-report-care-austria⁄